Maintenance is a long, steady, exhausting run. I'm sure I've said this in the blog before, but it bears repeating: If the first 8 months were a sprint, now we're running a marathon. Slow and steady wins the race. The thing is, during maintenance, nothing much happens. It's just month after month after month of exactly the same thing. As a result, there's not much to write about.
There have been a few things that I thought maybe I should have blogged about, but nothing big. Matthew is lactose intolerant now, as a result of his cancer treatment. We don't know if his tolerance for lactose will return to normal after treatment or not. Only time will tell. He's had some mysterious headaches that freak me out to the enth degree. I got a little bit crazy for a couple of months, mostly around those headaches. You see, this is the time when he is most likely to relapse -- from now until about a year after he stops treatment -- so I am on a constant alert for symptoms. It's like being filled with adrenaline all the time. Eventually, it gets to you. Matthew's poor doctor had to talk me down after a couple of months into my crazy time. They check for these things regularly, and the headaches would get progressively worse if they were an indicator of something sinister, not come and go. I just needed someone to reason with me. I guess it just feels like we're in a constant state of waiting for the other shoe to drop -- as if enough shoes haven't dropped. Also, we're always adjusting Matthew's oral chemo dose a little bit at a time. He has a tendency to run high on ANC, and we're always trying to suppress it just a titch more. Well, a couple of months ago, we overdid it, and his counts tanked. The result was that he became neutropenic and got to spend a few weeks confined indoors. He did not like that. I asked friends on Facebook to send cards, and he got "Christmas in the Mailbox" every day for about a week. People are amazing. He bounced right back from that, and went right back to his normal dose (without the upgrade we had tried to take) of oral chemo.
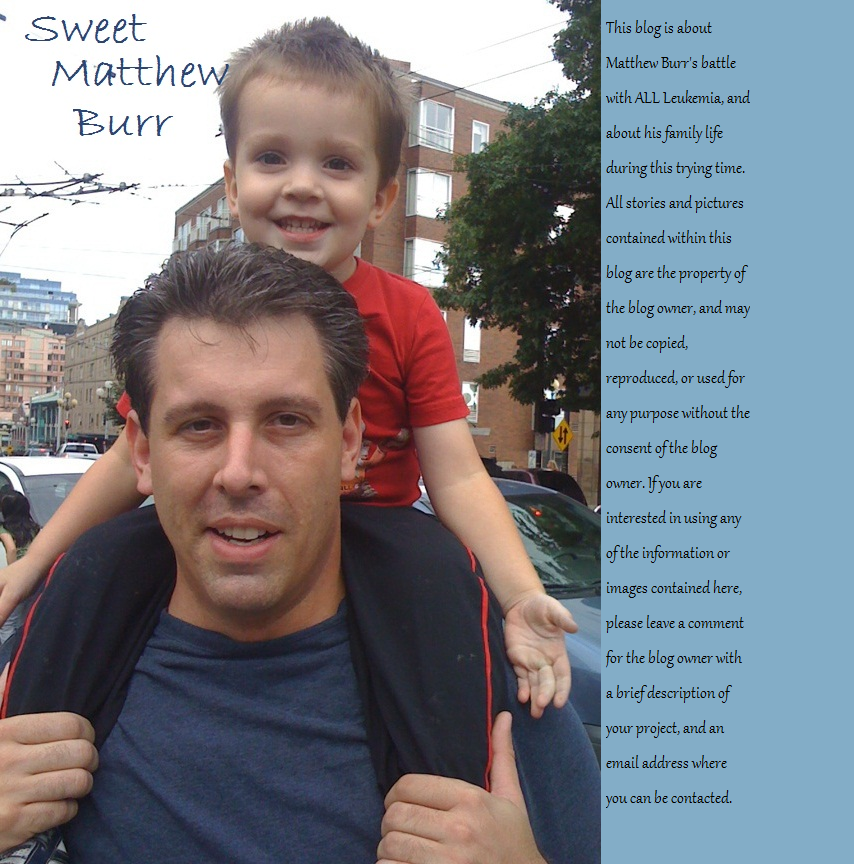
Matthew has this thing about him. He manages to get awful maladies, but then he is hardly affected by them. It's so strange. You would never look at him and know what he's going through or what he's gone through.
Well, another shoe dropped this week, and in true Matthew style, it's not as bad as I've always imagined it could be. I actually think it's not as bad as the doctors and nurses imagined it should have been. I say that because two different times, they acted very urgently about his well-being, and then they saw him, and they all sort of mellowed out. Quickly. Like someone had let the air out of a balloon.
I'm just going to tell the whole story, because I put little bits and pieces on Facebook, and I think I left some people confused.
Last Sunday (9 days ago, now), Matthew complained of a sore throat. He said it hurt him a lot to swallow. I'm far enough in nursing school to know that I should look, but not far enough to know what to do if I spot weird things. So I looked, and spotted something weird, and had no idea what to do. He had these red polka-dot like spots on the roof of his mouth, at the back, near his throat. The next day, he had a headache, runny nose, and a cough. I gave him benadryl to dry out his sinuses and sent him to school. That evening, he had a fever of 101.7, so I took him to the ER. The rule is that if the fever is above 101, we go to the ER. Even if it's just from a little cold. If I understand correctly, the reason is because he has a port, and a blood infection at the site of his port is too close to his heart for comfort. They have to be treated immediately.
So, for his little cold, we went to the ER. They gave him IV antibiotics (Rocephin), a bag of fluid, and checked his ANC. It was 2000, so we were clear to go home. But they ran a strep culture (rapid test was negative), a nose culture, and a blood culture. This is all standard every time he goes to the ER, right down to the same meds.
Tuesday, his fever was still above 100, so I kept him home from school. I called the clinic, and his nose culture had come back. Rhino virus and entero virus (which I found out later always come back together. It just means rhino virus. ... weird.) Matthew had the common cold.
Wednesday, his fever was gone, so I sent him to school. This had been enough trouble already for a cold. It was a totally normal day. He went and played at a friend's house after school and everything. Then, we put him to bed, and when I was getting ready for bed, I noticed a message on the answering machine. It was the ER. There was a concern about his blood culture. I should call them back. The message was from 4pm, but I didn't see it until about 10:30. I called them, and they said something had grown in his blood. We needed to come back to the ER. I asked should I wake him up or come in the morning? They said wake him up and come now. When we got there, they were urgent. Therefore, I worried. They didn't want to give him anything to eat or drink. I thought maybe his port was infected -- something that is always a worry in the back of my mind, because his port is right next to his heart. If that was the case, they would surgically remove it. In the beginning of his illness, I got the impression that we'd be lucky if we made it to the end with just one port, so I've been braced for it all along.
I'm going to interrupt here and say this. Blood infection is one of the things a cancer parent fears the most. Believe it or not, it can be even scarier than relapse. When we talk about kids dying because of their treatment, rather than the cancer, it's usually because of blood infection. They can cause sepsis, meningitis, or blood clots resulting in stroke or pulmonary emboli. If a kid in cancer treatment dies suddenly, it's likely that they had a blood infection. And just like you never think your own kid will be the one who gets cancer, once you're in that club, you think your kid will never get a blood infection. It's shocking when the ER staff tells you by phone to come now, even though it's the middle of the night, because there's something in his blood culture. Shocking and scary.
So, we went back up to the ER, they were urgent, and I was worried and scared. They put us right back into a room. No triage. Weird. And they gave him IV antibiotics again (Rocephin) and fluids. They took more blood for a new blood culture, and the doctor came and talked to me. She said that although they didn't know what it was yet, it was a gram negative bacilli. Basically, that just tells them how it responds to a certain die, and the shape of the bacteria. Sort of to help them classify it. She said that since Matthew didn't have any symptoms (even his cold symptoms were mostly resolved), we could go home, but we needed to follow up with oncology first thing in the morning. Strange, after all that build up. I took him home to stew over it there.
Thursday, I called oncology. At first, the phone call was very routine, but then I said they had found a gram negative bacilli in Matthew's blood, and the urgency set in. Again, that pit settled in my stomach. They wanted us to come up that day to meet with an infectious diseases doctor. We should pack a bag for an admit. Holy moly.
We got there, and they didn't want Matthew to eat. There was talk of scans. What were they scanning for, Justin asked. Oh, the doctor will come explain. It was overwhelming and new, sort of like when he first got sick The infectious diseases doctor (somehow, that's even scarier than oncologist) came in and explained that the bacteria in Matthew's blood is a very slow growing bacteria, so they still aren't sure what it is. They think it's a bacteria called fusobacterium. This is a normal bacteria that lives in all of our mouths. The sores at the back of Matthew's mouth on Sunday, combined with his immune compromised status, most likely allowed this bacteria to cross over into Matthew's blood stream. This is what the doctors have always warned us about. He couldn't even fight off the bacteria that lived in his own body. He couldn't fight them off, even with an ANC of 2000. That was a surprise to me, and I have spent 2 years educating myself as much as I can about these things.
Fusobacteria, once in the blood, is notorious for causing blood clots in the jugular or pulmonary emboli. If there's a blood clot in the jugular, it can "throw off" into the brain and cause a stroke. The scans the nurse had mentioned were CT scans to check for clots in the neck and lungs. This would determine our course of action. We were most likely looking at a 2-6 week admit.
Holy. Moly.

So, we went down and did the scans. Aaaand ... nothin. There was nothing on the scans. Totally clean. And since he still showed no symptoms related to this ailment, they decided that it would be okay for us to take him home, provided that we have home healthcare come to our house and teach us how to administer IV antibiotics.
Our fabulous nurse found us a home health company that was different than the last one we had out here (because they were not wonderful), and set it all up, and we were on our way. On the way home, I got a call from the home health care company, saying that they don't have nurses where we live, so they had to outsource. You guessed it ... to the sucky place we were trying to avoid. Sigh. So, then, they went on to tell me that they would be out first thing in the morning. Well, that wasn't okay, because he had a dose of antibiotics due at midnight. But I was told ... and I quote ... "Nursing doesn't happen in the middle of the night."
Uhhhh okay. We'll see you in the morning then. I guess.
And then I called the oncologist on call. I was 12 minutes late to reach someone at the clinic. They had just barely closed. The on call doctor said it was not okay to wait until morning, so she called the home health company back. There was a lot of back and forth, during which she said to pack up and come back, because we were being admitted until morning, but then the home health company miraculously figured out how to make nursing happen in the middle of the night.
If my writing is not thick with sarcasm, you should insert it above. I seriously do anything to avoid relying on home health care, because we have rarely had a good experience.
But, we got a huge delivery at about 9pm, and then as scheduled, we got a nurse at 11pm, who taught me how to prepare and administer Matthew's IV antibiotics. He was nice, too, and knew what he was talking about. Bonus. Then in the morning, another nurse came to observe me preparing and administering the antibiotics, to be sure I had it right. I did, and they said I was good to do it on my own.
Since then, we've been giving Matthew meropenem every 8 hours by IV. Justin learned how to do it, and we're working together so he can still work and I can still go to school. They gave us the okay today to send Matthew back to school tomorrow. His port will be accessed, but we'll just give the antibiotic in the morning and evening, and a dose in the middle of the night.
He did knock the port needle loose once, which he often does when he has to stay accessed for a long time. When Justin tried to flush it in the morning, he said it hurt, so we called the home health company. They sent us a nurse (who we recognized from before), and he tried to access the port, unsuccessfully. This guy bugs me a lot. He does things that I know he's not supposed to do, and he tries to access Matthew's port, when it's obvious that he doesn't know how, and every time, he claims that the port must be broken. So, we had to go up to primary's to have a nurse access him. Of course, the port is fine.
That makes 4 trips to the hospital and 3 visits from home health in a week. It's been crazy! But at least we're sleeping in our own beds.
Here's what we can expect. Thursday, the infectious diseases doctor said they were sending the blood samples to ARUP (a blood lab) for testing. She hoped we would know more by Monday (yesterday). What we have so far is that they still think it's fusobacterium in the first sample (from Monday in the ER), and that nothing has grown in Wednesday or Thursday's samples. This is good news all around. They're testing the infected sample for sensitivity to different drugs, in hopes of changing from meropenem every 8 hours to rocephin every 24 hours, but as of this afternoon, we didn't have results for the sensitivity tests. They said he can go to school tomorrow, as long as it doesn't interfere with his med schedule.
We should get more info tomorrow, but then again, maybe not. We'll see.
Thanks for the support and prayers! Blood infections can be so scary! But this is okay. We're stressed, but it's okay. Mostly we're really tired.
Captain Crunch and meropenem. The breakfast of champions.